In the United States, the healthcare system is perceived to be the key driver of health and health outcomes and usually serves as the focal point of efforts to improve health. However, transforming the healthcare delivery system in and of itself may not lead to the desired improvement in health outcomes. Research demonstrates that improving population health and achieving health equity also will require broader approaches that address social, economic, and environmental factors that influence health. The following graph looks at factors contributing to health status, demonstrating that healthcare interventions alone have far less impact than a combination of environmental and social factors. 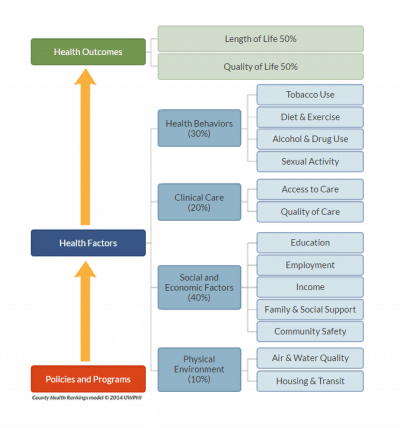
How then do we in the healthcare setting work effectively to improve health outcomes at the population level? Healthcare organizations must work in collaboration with community organizations to ensure that patients have access to resources addressing the social determinants of health. The official term for this network of community partners is the “Medical Neighborhood,” defined by the Patient-Centered Primary Care Collaborative as “a clinical-community partnership that includes the medical and social supports necessary to enhance health. The goals… include collaborating with these various “medical neighbors” to encourage the flow of information across and between clinicians and patients, to include specialists, hospitals, home health, long term care, and other clinical providers, along with non-clinical partners like community centers, faith-based organizations, schools, employers, public health agencies, YMCAs, and Meals on Wheels. Together these organizations can actively promote care coordination, fitness, healthy behaviors, proper nutrition, as well as healthy environments and workplaces. A successful medical neighborhood will “focus on meeting the needs of the individual patient, but also incorporate aspects of population health and overall community health needs.” https://www.pcpcc.org/content/medical-neighborhood
Through quality initiatives designed to facilitate transformation among physician practices, CMS acknowledges this need for clinical and non-clinical partnership in communities, incorporating milestones into these initiatives that guide physician practices to begin to function as part of a Medical Neighborhood:
- Community Resource Referrals – this milestone encourages practices to:
- Facilitate referrals to appropriate community resources, including community organizations and agencies as well as direct care providers
- Maintain a documented list of community resources that is appropriate for their patient population, and easily accessible for both the clinical and non-clinical staff to provide to the patient
- Document this information in the electronic medical record
- Complete training to enable staff to identify the indicators for patient need
- Medical Neighborhood – this milestone encourages practices to:
- Work with the primary care practices in its medical neighborhood to develop criteria for referrals for:
- episodic care
- co-management
- transfer of care/ return to primary care
- processes for care transition, including communication with patients and family
- Develop personal and electronic relationships among medical neighborhood providers to ensure information sharing
- Assign responsibility to specific staff members for care coordination and referral management
- Work with the primary care practices in its medical neighborhood to develop criteria for referrals for:
Based on discussions about the Medical Neighborhood concept with physician practices, the uptake may be slow. Practices regularly make referrals to other providers, but development of relationships and formalized processes for making referrals to non-clinical, community-based organizations and ensuring closed-loop communication to ensure the patient follows up on the referral is new to some. One pediatrician offered the opinion that one practice can’t create a Medical Neighborhood by themselves where none exists, which underscores the need to provide physician practices with instruction on how to establish community partnerships as a critical component of transformation. How do physician practices go about establishing these community partnerships to facilitate achievement of these milestones?
- Select the Target population – Physician practices are recommended to target a patient population that is at a high risk for hospital readmissions. Typically, these patients also have non-clinical issues contributing to their health condition that could be impacted positively by appropriate community resource referrals.
- Assess Non-Clinical Needs of the patient population
- Identify Community Resources – Determine which resources are available in the community to make an impact on the non-clinical needs of the patient population
- Form partnerships – through MOAs, MOUs, joining an existing community coalition, practices need to develop relationships with organizations that can provide the patient population with needed resources
- Develop Strategies / Processes – Within the practice, determine processes for documentation of patient indicators, reviewing / flagging risk, and referrals given and followed up in the EMR. Within the neighborhood, determine processes for referral communication and information sharing. Also, innovative strategies could be considered involving the physician practice and community partners, such as “produce prescriptions” and discounts to fitness classes for diabetic patients.
- Monitor Results – information about referrals and patient follow-up, and impact on associated health outcomes is tracked in EMR, and progress is monitored and reported.
When I have asked physicians and practice managers why their practices have chosen to engage in the transformation effort, the reason frequently given is to maximize reimbursement (and minimize penalty). While this is accurate and penalties certainly will become increasingly significant over the next few years, I believe that a focus on metrics obscures the greater goal of healthcare transformation. As physician practices authentically transform as they achieve these milestones, they will achieve improved quality and reduced costs as a by-product of their transformation efforts. The vision of CMS is to form medical neighborhoods across the country as physician practices collaborate with one another and other clinical and non-clinical organizations in their communities to manage risk and help individuals in those communities to achieve their best health.
###
For more information, contact Anne Nita at anne.nita@staging.infoworks-tn.com.