There seems to be an increased amount of news highlights and articles about challenges serving patients in behavioral health. It has caused me to wonder, “why now?” Behavioral health encompasses historically stigmatized conditions like substance addiction and abuse as well as psychological distress and mental disorders. Perhaps the chatter about behavioral health is in part tied to the current opioid epidemic and how to stop opioid abuse. There has also been a lot of coverage and shocking statistics have surfaced related to opioid-related deaths and the increased numbers of babies being born addicted to narcotics. One in five people will be diagnosed with a mental illness and drug overdose is now the #1 cause of death in the United States.
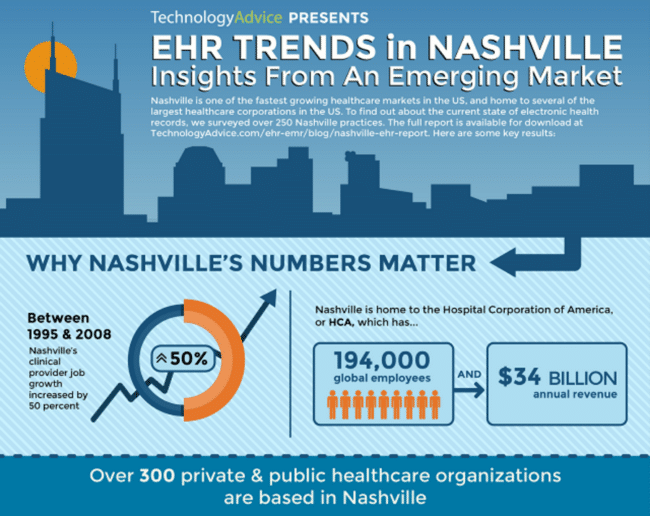
Seeking to learn more, I attended a Leadership Healthcare (LHC) Fundamentals Series on Behavioral Health last month that included panelists representing TennCare, HCA Behavioral Health Services, Acadia Healthcare, and the Tennessee Department of Mental Health and Substance Abuse Services. The TennCare panelist shared a staggering statistic that Tennessee has experienced a 10-fold increase in babies being born with neonatal abstinence syndrome in the last 10 years.
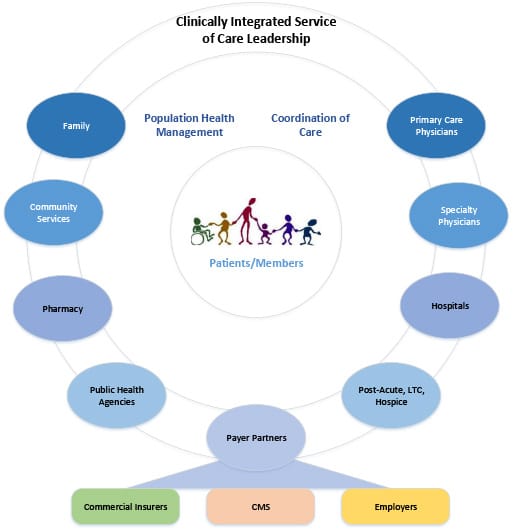
Regardless of the specific reasons around addiction or abuse, I’m optimistic about the increased focus on behavioral health as it is a needed component of care delivery. Behavioral health conditions can actually delay progress in therapies when treating a co-morbidity, such as a cardiac condition. I think it is one of the fields that could benefit most from advances in technology and new care delivery models that we are already applying in other healthcare specialties. Early in the LHC session, all four speakers identified access as a key issue in the behavioral health space. For those seeking treatment, it is difficult to find affordable, outpatient options. A compounding factor is that behavioral health is a field that also experiences a shortage of doctors in America. The Kaiser Family Foundation estimates that less than 50% of the need is met in America for psychiatrists. That is a significant gap and growing over time. How could technology advances help close this gap?
I learned through the LHC session that HCA is exploring an approach that I believe could help solve this issue and others: telepsychiatry. In my opinion, mental health exams are the perfect candidate for telemedicine, as I understand they can be conducted without physically touching the patient. Psychiatric consultations have been delivered through telemedicine since the 1950’s. Telemedicine can fill many of the gaps in behavioral health delivery, such as specialist coverage, for mental health assessments before transitioning a patient to another care setting or assessing co-morbidities in emergency room triage like HCA is doing in some areas. Telemedicine delivery would also enable a client to receive treatment with an increased degree of privacy, if that is a concern. It also might combat the psychiatrist shortage in affected areas by virtually connecting psychiatrists from another part of the country to patients in need.
I’m encouraged by stories like the HCA creative approaches. I am currently working with a behavioral health vendor that is looking to automate some processes with electronic records and is considering telemedicine for future projects. This session enabled me to bring back some specific ideas to this client to help them evolve their concepts and think a little more outside the box to leverage technology more effectively.
Now that we have the technology and adoption is on the rise, it’s time to turn our focus to application in the populations that need it the most and behavioral health is a great candidate with accelerating gaps in coverage and number of patients needing intervention.