As organizations dip their toe in the water of Clinically Integrated Systems of Care, or expand from a strong foundation, it is important to understand that these new care delivery models are not typically competitive and are usually not mutually exclusive. In fact, each are highly complementary. For example, a successful Accountable Care Organization (ACO) has at its core a network of independent physicians who share common goals driven by improving the quality of care for their patients through more efficient models. Clinical integrated networks (CIN) improve overall performance and experience of care for their patients and members via Patient Centered Medical Home (PCMH) principles and practices.
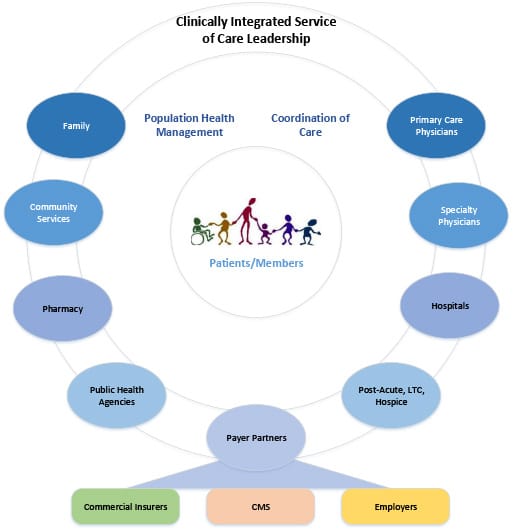
Clinically Integrated Systems of Care also share core components required for long term sustainability, see Figure 1.
Figure 1 Source: Becker’s Hospital Review
- Physician engagement and leadership – In all models, clinical decision making is core to the operations. As such, these models rarely succeed if physicians are not engaged from the start to participate or lead development of goals and objectives.
- Performance and improvement measures and metrics – Although each of the care delivery models discussed can operate in existing fee-for-service incentive structures, they all imply, and typically define, specific criteria for a pay-for-performance incentive structure. For certain procedures, this will quickly evolve to 100% risk-based models by 2016.
- Funds flow – Calculation and distribution of funds to all healthcare partners engaged in the system must be defined, transparent, and easy-to-understand for long-term engagement and sustainability.
- Information technology and data management – Interoperability and data sharing are essential across all partners in the clinically integrated system, enabling all providers to complete eligibility, benefits, clinical history, and clinical decision details. The goal is two-way data sharing across all medical devices, EHRs, population health systems, and value-added applications.
Opportunity: From a Consumer or Patient’s Perspective
In many cases, these Clinically Integrated Systems of Care yield provider, patient, and member experiences that feel more authentic than traditional care delivery as a result of collaboration and common goals and objectives. The opportunity is to consider the ‘outside-in’ view of a consumer, member, or patient’s perspective when communicating to these audiences. Even explaining what a ‘medical home’ is in terms of what exists today is a challenge. If I am a fairly healthy consumer who only sees a primary care physician annually for a well check-up, do I have an incentive to change to a medical home? Will I have to change? If my primary communication device is a smartphone and English is not my primary language, how will a medical home help me? Successful organizations will first segment consumers and patients before determining communication strategies. Potential segmentation aspects include the following areas: demographic and ethnic related data, insurance plan type combined with ability to pay out of pocket, and level of health status from mostly healthy to complex, chronic care management.